Ever wonder how doctors and healthcare providers get approved to work with insurance companies? It’s not as simple as applying for a job and showing up to work. That’s where Provider Credentialing Services come in.
Think of credentialing like getting a backstage pass. Without it, providers can’t access the stage—that is, treat patients under insurance plans. Whether you’re a patient curious about your provider’s legitimacy, or a clinic owner searching for a medical billing company near me to streamline your processes, this guide is here to clear the fog.
Let’s break it all down together—no jargon, no fluff.
1. What is Provider Credentialing?
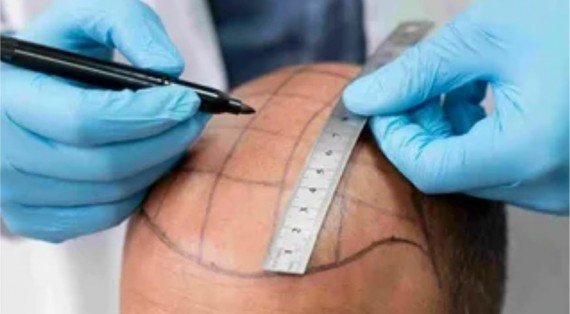
Provider credentialing is the process of verifying the qualifications, training, and professional history of a healthcare provider. It’s like running a background check, but specific to medicine—making sure the provider is legit and trustworthy.
2. Why is Credentialing Important?
Imagine getting surgery from someone without proper qualifications—scary, right? Credentialing helps prevent that. It protects patients and ensures providers meet industry standards. Also, insurance companies require it before reimbursing providers.
Without credentialing, providers can’t get paid. Period.
3. Who Needs Credentialing?
Basically, anyone who treats patients and wants to accept insurance must go through this process. This includes:
- Doctors
- Nurse practitioners
- Therapists
- Chiropractors
- Dentists
Even small practices need credentialing if they want to be in insurance networks.
4. How Does the Credentialing Process Work?
Think of it like building a puzzle:
- Application submission – Providers send their qualifications to insurance companies or hospitals.
- Verification – The information is checked and double-checked.
- Approval – Once verified, the provider is added to the network or facility.
This process involves tons of paperwork and back-and-forth communication.
5. The Role of a Medical Billing Company in Credentialing
You may ask: “Can’t we do this in-house?” Sure, but it’s like fixing your car when you’re not a mechanic—possible, but not efficient.
That’s why many clinics turn to a medical billing company near me. These companies handle the grunt work:
- Submitting documents
- Following up with insurers
- Fixing errors
- Managing renewals
This frees up your staff and keeps things running smoothly.
6. Common Documents Required
Here’s what’s usually needed:
- Medical license
- DEA certificate
- Board certifications
- Malpractice insurance
- CV or resume
- Work history
- References
Forget one, and your application can get delayed for weeks.
7. Typical Timeline for Credentialing
So, how long does it take?
Usually, 60–120 days. It depends on:
- How quickly documents are submitted
- Insurance company response times
- Whether there are any red flags
Delays happen often if you don’t stay on top of it.
8. What Happens if Credentialing is Delayed?
Delays are costly. Here’s what can go wrong:
- You can’t see patients under insurance plans
- Claims get denied
- You lose revenue
In a worst-case scenario, you might even face legal penalties for billing without approval.
9. Recredentialing – What is it and Why it Matters
Credentialing isn’t one-and-done. Every 2-3 years, providers must recredential to stay in good standing.
Think of it like renewing your driver’s license. If it expires, you’re out of commission.
10. Benefits of Outsourcing Credentialing Services
Why do smart clinics outsource?
- Expert handling – Trained professionals manage the process.
- Faster approvals – Fewer delays mean quicker patient access.
- Error-free submissions – Avoid rejections.
- Better follow-up – You don’t have time to chase insurers—let the experts do it.
A professional medical billing company near me is like hiring a GPS for your credentialing journey.
11. Choosing the Right Credentialing Partner
Not all services are created equal. When picking a credentialing partner:
- Check reviews and testimonials
- Ask about turnaround times
- Understand their pricing model
- Confirm they offer ongoing support
- Look for experience in your specialty
Pro tip: Choose one that also offers billing services to simplify your workflow.
12. How Credentialing Affects Medical Billing and Payments
Here’s the deal: No credentialing = no billing.
Even if you see a patient, if you’re not credentialed, the insurance company won’t pay you. It’s like trying to use a canceled credit card—it won’t work.
Credentialing ensures that claims are accepted and reimbursed without issues.
13. Challenges in the Credentialing Process
Credentialing is a pain for a reason. Common challenges include:
- Missing or outdated documents
- Delays from insurance companies
- Human error in forms
- Not following up promptly
- Miscommunication between providers and payers
And if you’re doing it alone? Multiply that stress by ten.
14. Tips to Speed Up the Credentialing Process
Want things to move faster? Follow these tips:
- Gather all documents beforehand
- Use checklists to stay organized
- Respond quickly to requests
- Set reminders for license renewals
- Use a reliable medical billing company near me
Remember, time is money—especially in healthcare.
15. Final Thoughts and Takeaways
Credentialing might seem like a headache, but it’s a necessary part of running a successful practice. Whether you’re a solo provider or managing a multi-specialty clinic, getting credentialed—and staying that way—is key to keeping your doors open and your revenue flowing.
Partnering with a professional for provider credentialing services can take the burden off your shoulders, save you time, and help you get paid faster. If you’re looking for a medical billing company near me, now is the perfect time to find one that offers complete support—including credentialing.














Leave a Reply